Does Exercise Induce Your Migraines?
And even if exercise doesn’t trigger your migraines…
What follows is still highly relevant. Many migraine sufferers share a similar internal landscape: impaired methylation, elevated homocysteine, and poor histamine clearance—regardless of what their specific trigger is. So whether your migraines are brought on by stress, certain foods, hormonal shifts, or weather changes, understanding and optimizing these core biochemical pathways can significantly reduce frequency and intensity—and may even eliminate them altogether.
Unraveling the Link Between MTHFR, Homocysteine, Histamine, and Head Pain
If you’ve ever been told that exercise is good for you—but it keeps triggering migraines—you’re not alone, and you’re not imagining things. For some people, physical exertion isn’t energizing—it’s the spark that ignites a chain reaction in the body, ending in a migraine that can derail your day (or longer). But why?
The answer may lie in your genetics, your biochemistry, and a hidden trio of internal imbalances: MTHFR mutations, elevated homocysteine, and histamine overload.
Let’s unpack what’s really going on beneath the surface.
MTHFR: The Gene That Shapes Your Methylation Pathways
MTHFR stands for methylenetetrahydrofolate reductase—an enzyme critical for your body’s methylation process. Methylation impacts everything from detoxification to neurotransmitter balance to energy production. It’s also the key process that allows your body to convert homocysteine (a potentially toxic amino acid) into methionine, a vital building block for health.
But here’s the issue: up to 40–60% of people carry a mutation in the MTHFR gene (most commonly C677T or A1298C) that reduces methylation efficiency. If you carry one of these variants, your body struggles to:
- Properly activate folate (into 5-MTHF)
- Recycle homocysteine
- Methylate histamine
That dysfunction has downstream effects, especially for migraine sufferers.
Homocysteine: A Hidden Trigger for Neurovascular Stress
When methylation is sluggish, homocysteine builds up in the blood. And elevated homocysteine isn’t just a cardiovascular risk factor—it’s neurotoxic and inflammatory. It increases oxidative stress, irritates the blood vessels, and affects the delicate balance of cerebral blood flow.
This is important because migraine is, at its core, a neurovascular condition.
When homocysteine is high, it can:
- Trigger the constriction and dilation of cerebral arteries
- Sensitize pain receptors
- Create the ideal conditions for a migraine to take hold—especially under the added stress of exercise
- Histamine in the brain can also be the cause of brain fog.
Histamine: The Underestimated Migraine Molecule
Histamine is best known for its role in allergies, but it’s also a potent neuromodulator. It influences the brain, gut, immune system, and vascular tone. And here’s the connection: histamine needs methylation to be broken down.
In the brain and liver, histamine is cleared via HNMT (histamine-N-methyltransferase)—an enzyme that depends on methyl groups supplied by the same pathway impacted by MTHFR mutations.
If methylation is sluggish:
- Histamine isn’t broken down efficiently
- It accumulates in the brain and body
- You become more reactive to histamine-liberating foods and activities—including exercise
Even worse, exercise itself increases histamine release, as your body ramps up blood flow and immune response. So if you’re already histamine-sensitive, exercise can push you over the edge into migraine territory.
And it’s not just migraines—brain histamine affects your cognition and sleep, too.
In the brain, histamine acts as a wakefulness-promoting neurotransmitter. When levels are too high—often due to poor methylation or impaired histamine breakdown—it can lead to brain fog, restlessness, and insomnia. Many people with histamine intolerance report trouble focusing, racing thoughts at night, or waking up frequently. If you’re experiencing these symptoms along with migraines, it’s another clue that histamine and methylation may be at the root.
Why Exercise Triggers Migraine in Sensitive Individuals
Let’s connect the dots:
- You have an MTHFR mutation → reduced methylation
- Methylation is needed to lower homocysteine and clear histamine
- Homocysteine irritates blood vessels and the brain
- Histamine builds up, making you more sensitive to stimuli
- Exercise liberates even more histamine, increases nitric oxide, and activates an already overstimulated system
Result? Boom: Migraine.
What You Can Do: Functional Strategies That Help
If this is your pattern, you’re not stuck. You just need to optimize your internal terrain. Here’s how:
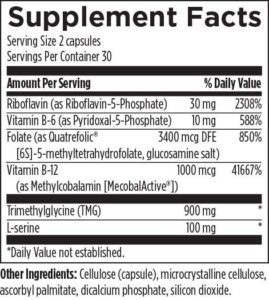
1. Support Methylation
- 5-MTHF (activated folate): 400–1,000 mcg daily
- Methylcobalamin (Vitamin B12): 1,000–5,000 mcg as needed
- Riboflavin (Vitamin B2) and P5P (Vitamin B6) to support cofactor needs
- TMG (trimethylglycine) or SAMe in some cases
2. Lower Homocysteine
- The above nutrients help
- Add magnesium, zinc, and choline as needed
- Aim for homocysteine between 6–8 µmol/L
Clinically Formulated Support: One of the most comprehensive ways to support methylation and lower homocysteine is with a well-balanced supplement like Homocysteine Supreme® by Designs for Health, which combines activated B vitamins, TMG, and supportive cofactors in clinically effective doses—all in one formula.
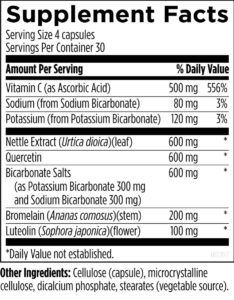
3. Manage Histamine
- Try a low-histamine diet temporarily, if this helps it is a good indication that histamines are playing a role.
- Avoid known liberators: alcohol, aged cheese, fermented foods, intense exercise during flares
- Consider DAO enzyme before meals or exertion
- Use mast cell stabilizers like quercetin, luteolin, or vitamin C (all 3 are found in HistEze)
4. Stabilize the Brain
- Magnesium glycinate or threonate for neurovascular calm
- CoQ10 for mitochondrial support
- Omega-3s to reduce inflammation
- Prioritize sleep, hydration, and steady blood sugar
If you’re experiencing migraines after exercise, the issue might not be the exercise—it might be your biochemistry.
MTHFR mutations, high homocysteine, and poor histamine clearance often go undiagnosed—but they set the stage for a sensitive, reactive system. When you add the physical stress of a workout to that terrain, it can trigger migraines that seem mysterious but are entirely biologically explainable.
With targeted support—like methylation nutrients, histamine management (HistEze & a low histamine diet), and DAO enzyme supplementation—you can shift the terrain, support your nervous system, and experience what exercise is truly meant to provide: energy, resilience, and vitality.
Reference List
- MTHFR Function and Mutations
- Frosst, P., Blom, H. J., Milos, R., Goyette, P., Sheppard, C. A., Matthews, R. G., … & Rozen, R. (1995). A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nature Genetics, 10(1), 111–113.
https://doi.org/10.1038/ng0595-111 - Methylation and Homocysteine Metabolism
- Mudd, S. H., Finkelstein, J. D., Refsum, H., Ueland, P. M., Malinow, M. R., Lentz, S. R., … & Wilcken, B. (2000). Homocysteine and its disulfide derivatives: a suggested consensus terminology. Arteriosclerosis, Thrombosis, and Vascular Biology, 20(7), 1704–1706.
https://doi.org/10.1161/01.ATV.20.7.1704 - Homocysteine and Migraine
- Oterino, A., Valle, N., Bravo, Y., Muñoz, P., Alonso-Arranz, A., Castillo, J., & Pascual, J. (2004). MTHFR T677 homozygosis influences the presence of aura in migraineurs. Cephalalgia, 24(6), 491–494.
https://doi.org/10.1111/j.1468-2982.2004.00711.x - Homocysteine and Endothelial Dysfunction
- Welch, G. N., & Loscalzo, J. (1998). Homocysteine and atherothrombosis. New England Journal of Medicine, 338(15), 1042–1050.
https://doi.org/10.1056/NEJM199804093381507 - Histamine Metabolism and Methylation (HNMT pathway)
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American Journal of Clinical Nutrition, 85(5), 1185–1196.
https://doi.org/10.1093/ajcn/85.5.1185 - DAO Function and Histamine Clearance
- Schwelberger, H. G. (2004). Histamine intolerance: a metabolic disease? Inflamm Res, 53(S1), S49–S50.
https://doi.org/10.1007/s00011-004-0331-1 - DAO Enzyme Expression and Supplementation
- Mušič, E., & Šilar, M. (2013). Diamine oxidase and its role in histamine metabolism. Biomedicine & Pharmacotherapy, 67(2), 139–144.
https://doi.org/10.1016/j.biopha.2012.11.013 - Exercise and Histamine Release
- Stokes, K. Y., & Granger, D. N. (2005). The microcirculation: a target for histamine in health and inflammation. Journal of Allergy and Clinical Immunology, 115(4), 739–747.
https://doi.org/10.1016/j.jaci.2004.11.048 - Histamine-Induced Migraine Mechanisms
- Wantke, F., Gotz, M., & Jarisch, R. (1993). Histamine-free diet: treatment of choice for histamine-induced food intolerance and migraine. Clinical and Experimental Allergy, 23(12), 982–985.
https://doi.org/10.1111/j.1365-2222.1993.tb03379.x - Histamine and Vasodilation
- Masini, E., Blandina, P., Vannacci, A., & Mannaioni, P. F. (2000). Histamine and inflammation: from basic science to clinical aspects. Pharmacological Research, 41(5), 361–368.
https://doi.org/10.1006/phrs.1999.0619 - Quercetin and Mast Cell Stabilization
- Kimata, M., Inagaki, N., & Nagai, H. (2000). Effects of luteolin and other flavonoids on IgE-mediated allergic reactions. Planta Medica, 66(01), 25–29.
https://doi.org/10.1055/s-2000-11117 - Functional Strategies and Supplement Support
- Kennedy, D. O. (2016). B vitamins and the brain: mechanisms, dose and efficacy—a review. Nutrients, 8(2), 68.
https://doi.org/10.3390/nu8020068